PTE surgery
The treatment of choice for CTEPH
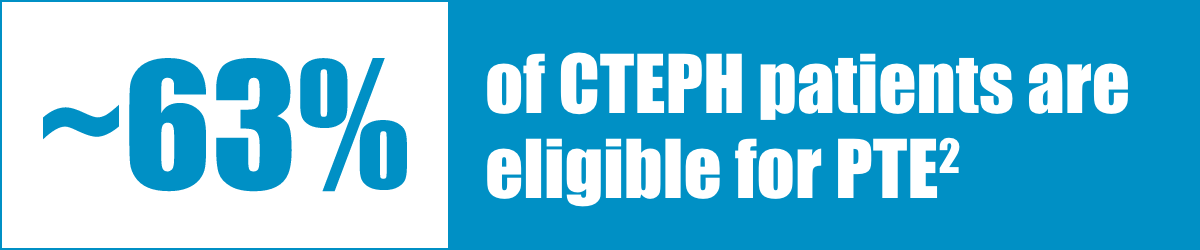
Pulmonary thromboendarterectomy (PTE) surgery (also called pulmonary endarterectomy [PEA]) is the only treatment for CTEPH that can be curative, so it is the recommended first option for CTEPH patients.1 According to an International Prospective Registry, approximately 63% of CTEPH patients are operable.2
PTE should be offered to all eligible patients with CTEPH. Most patients experience significant improvements in symptoms and hemodynamics.2-4 The international registry of incident cases of CTEPH reported a 3-year survival of 90% in those receiving PTE versus 70% in those who did not have surgery.3
Patients who have operable CTEPH should be referred for surgery without delay5
- PTE surgery is a complex bilateral procedure, which requires median sternotomy, cardiopulmonary bypass, deep hypothermia, and periods of circulatory arrest6
- PTE allows for the removal of obstructing lesions, resulting in an improvement and often normalization of pulmonary hemodynamics7,8
- Rates of residual pulmonary hypertension (PH) following PTE have been reported at 10% to 35%9-11


BPA may also be considered for technically operable patients with a high proportion of distal disease and an unfavorable risk: benefit ratio for PEA.3
Watch a real PTE surgery
Cameron Wright, MD, of Massachusetts General Hospital performs pulmonary thromboendarterectomy (PTE) on a patient with CTEPH.
Compensated by Bayer for video.
Post-operative follow-up
- Early reocclusion prophylaxis using intravenous or subcutaneous heparin and subsequent lifelong anticoagulation is mandatory for all patients following PTE surgery1
- Hemodynamic benefits may be seen immediately after surgery, but maximum benefits may not be observed for 6 months or longer1
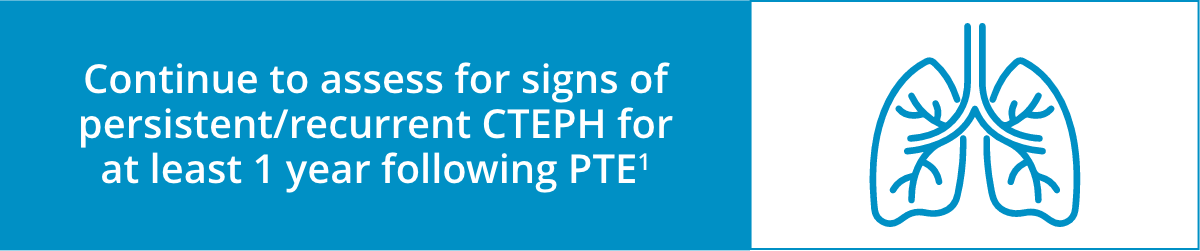
- Hemodynamic reevaluation should be conducted 6–12 months after surgery to exclude recurrent or residual symptomatic CTEPH1
- Treatment with vasodilators may be beneficial for recurrent or residual CTEPH1
Following PTE, patients must be closely monitored and reassessed regularly.1 Up to one-third of patients may have residual CTEPH following PTE.9 Therefore, physicians should remain vigilant in assessing for signs of persistent/recurrent CTEPH for at least 1 year following surgery.1 Continuity of care between the pulmonary specialist and primary care physician is essential during this crucial time period.
Post-PTE Surgery Follow-Up
Discover how CTEPH patients should be treated after undergoing PTE surgery.
Compensated by Bayer for video.
Post-PTE Surgery Discussion Guide for Patients
Give this useful guide to your PTE patients to help them assess and report their progress after PTE surgery.
References:
1. Keogh AM, Mayer E, Benza RL, et al. Interventional and surgical modalities of treatment in pulmonary hypertension. J Am Coll Cardiol. 2009;54(suppl 1):S67-S77. 2. Pepke-Zaba J, Delcroix M, Lang I, et al. Chronic thromboembolic pulmonary hypertension (CTEPH): results from an international prospective registry. Circulation. 2011;124(18):1973-1981. 3. Humbert M, Kovacs G, Hoeper MM, et al. 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022;43(38):3618-3731. 4. Kim NH, D'Armini AM, Delcroix M, et al. Chronic thromboembolic pulmonary disease. Eur Respir J. 2024;64(4):2401294. 5. Kim NH, Delcroix M, Jenkins DP, et al. Chronic thromboembolic pulmonary hypertension. J Am Coll Cardiol. 2013;62(suppl D):D92-D99. 6. Jamieson SW, Kapelanski DP, Sakakibara N, et al. Pulmonary endarterectomy: experience and lessons learned in 1,500 cases. Ann Thorac Surg. 2003;76(5):1457-1464. 7. Piazza G and Goldhaber SZ. Chronic thromboembolic pulmonary hypertension. N Engl J Med. 2011;364:351-360. 8. Rahnavardi M, Yan TD, Cao C, et al. Pulmonary thromboendarterectomy for chronic thromboembolic pulmonary hypertension: a systematic review. Ann Thorac Cardiovasc Surg. 2011;17(5):435-445. 9. Freed DH, Thomson BM, Berman M, et al. Survival after pulmonary thromboendarterectomy: effect of residual pulmonary hypertension. J Thorac Cardiovasc Surg. 2011;141(2):383-387. 10. Wittine LM and Auger WR. Chronic thromboembolic pulmonary hypertension. Curr Treat Options Cardiovasc Med. 2010;12:131-141. 11. Mayer E, Jenkins D, D’Armini A, et al. Surgical management and outcome of patients with chronic thromboembolic pulmonary hypertension: results from an international prospective registry. J Thorac Cardiovasc Surg. 2011;141(3):702-710.