BPA for CTEPH
BPA has become an established non-surgical intervention
Percutaneous balloon pulmonary angioplasty (BPA) may be an option for some patients who are not eligible for pulmonary thromboendarterectomy (PTE) surgery or have recurrent/persistent pulmonary hypertension following PTE.1 BPA has become an established treatment for such patients but should be reserved for expert centers with extensive training and experience.2,3
BPA opens obstructed vessels or widens stenotic lesions using a catheter-based intervention in order to restore pulmonary blood flow.1
BPA has been reported to improve3
- Hemodynamics
- Symptoms
- Exercise capacity
- Right ventricular function
BPA is recommended in patients who are technically inoperable or have residual PH after PTE and distal obstructions amenable to BPA.2 In patients who are candidates for BPA, approved medical therapy may also benefit the patient and should be considered in conjunction with BPA.2,3
BPA leads to significant improvements of pulmonary hemodynamics and physical capacity, with 3-year survival rates of 92% to 95%.3
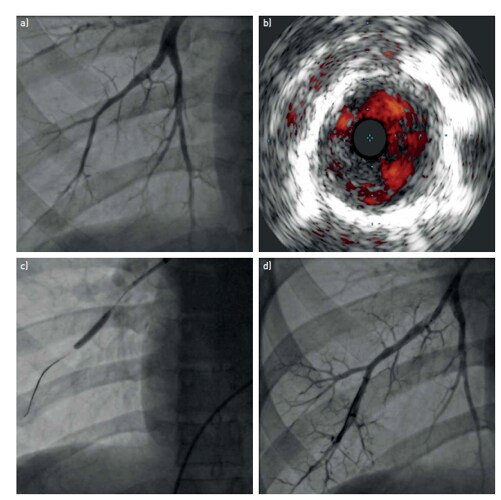
Pulmonary arterial imaging before and after percutaneous balloon pulmonary angioplasty (BPA).
a) Pre-procedure pulmonary angiogram demonstrating an intra-arterial fibrous “web” lesion; b) the corresponding intravascular ultrasound image showing the intravascular filling defect; c) the BPA balloon in place; d) pulmonary angiogram after the BPA procedure, showing the patent arterial lumen. Image from Lang et al 2017.1
Patients should be evaluated for BPA only at an expert center
BPA is a complex procedure that includes risk of complications and often requires multiple sessions. BPA requires extensive training and case experience, and should be reserved for expert centers with a CTEPH team.1-3
BPA should be considered for symptomatic patients who are ineligible for PEA due to distally localized pulmonary artery lesions or patients with persistent/recurrent PH after surgery. Therefore, the multidisciplinary team (MDT) is considered obligatory for decision-making.3
BPA should not be considered for patients with large central clots or unilateral total occlusion.1
Adapted from ESC/ERS Guidelines for Diagnosis and Treatment of Pulmonary Hypertension. 2022.
aSelected symptomatic patients with CTEPD without PH can also be treated by PEA and BPA. bMDT meeting can be virtual. cTreatment assessment may differ, depending on the level of expertise in PEA and BPA. dFor inoperable patients with PVR >4 WU, medical therapy should be considered prior to BPA; there are limited data on BPA as first-line therapy.
BPA = balloon pulmonary angioplasty; CTEPD = chronic thromboembolic pulmonary disease; CTEPH = chronic thromboembolic pulmonary hypertension; MDT = multidisciplinary team; N = no; PAH = pulmonary arterial hypertension; PEA = pulmonary endarterectomy; PH = pulmonary hypertension; PVR = pulmonary vascular resistance; WU = Wood units; Y = yes.
Complications with BPA
Complications include1:
- Hemoptysis
- Wire injury
- Vessel dissection
- Vessel rupture
- Reperfusion pulmonary edema
- Pulmonary parenchymal bleeding
- Hemorrhagic pleural effusions
Investigators have refined BPA by using smaller balloons and limiting the number of balloon inflations per session to 1 to 2 pulmonary vascular segments. Targeting only one lobe during each session and cautious balloon sizing have reduced the incidence of RPE to 2% in individual centers.4
For patients who are not candidates for PTE or BPA, approved medical therapy is recommended.2,3
References:
1. Lang I, Meyer BC, Ogo T, et al. Balloon pulmonary angioplasty in chronic thromboembolic pulmonary hypertension. Eur Respir Rev. 2017;26:160119. 2. Humbert M, Kovacs G, Hoeper MM, et al. 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022;43(38):3618-3731. 3. Kim NH, D'Armini AM, Delcroix M, et al. Chronic thromboembolic pulmonary disease. Eur Respir J. 2024;64(4):2401294. 4. Galie N, Humbert M, Vachiery J, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2016;37(1):67-119.